Spotlight Interview: Perinatal Peer Support Project Continues Post-Grant
While suffering crushing post-natal depression after the birth of her first child, Ashleigh Allan relied heavily on informal support from her peers – other mothers who had been through similar experiences.
Ashleigh’s child is now nine years old, but she hasn’t forgotten how important it was to her to have a dedicated support system during those difficult months. Recognising a gap in the professional services offered to women in her position, she has turned her own struggles into a positive as the first perinatal mental health peer worker appointed in NSW, committed to expanding the role to help more women in the South Eastern Sydney Local Health District (SESLHD) and beyond as they adjust to pregnancy and new motherhood.
Ashleigh began her journey of recovery and advocacy by connecting with Perinatal Anxiety & Depression Australia (PANDA). “Reading the lived experience stories on their website and hearing what other people had been through showed me that I wasn’t alone,” Ashleigh explains. “When I was in the depths of my experience, that little glimmer of hope that other women have been here and have come out the other side helped me believe I would be able to do that as well.” That prompted her to “think about what [perinatal peer support] could actually look like within services in a formal capacity.”
Perinatal mental health sits at the intersection of mental health and wellbeing, and the transitional experience of parenthood, Ashleigh says. Addressing the shift in self-identity, individual experiences of childhood and parenting, experiences of trauma, and personal and sociocultural expectations compared to reality, are all part of the perinatal peer support worker role, bridging the gap between clinical services and community support.
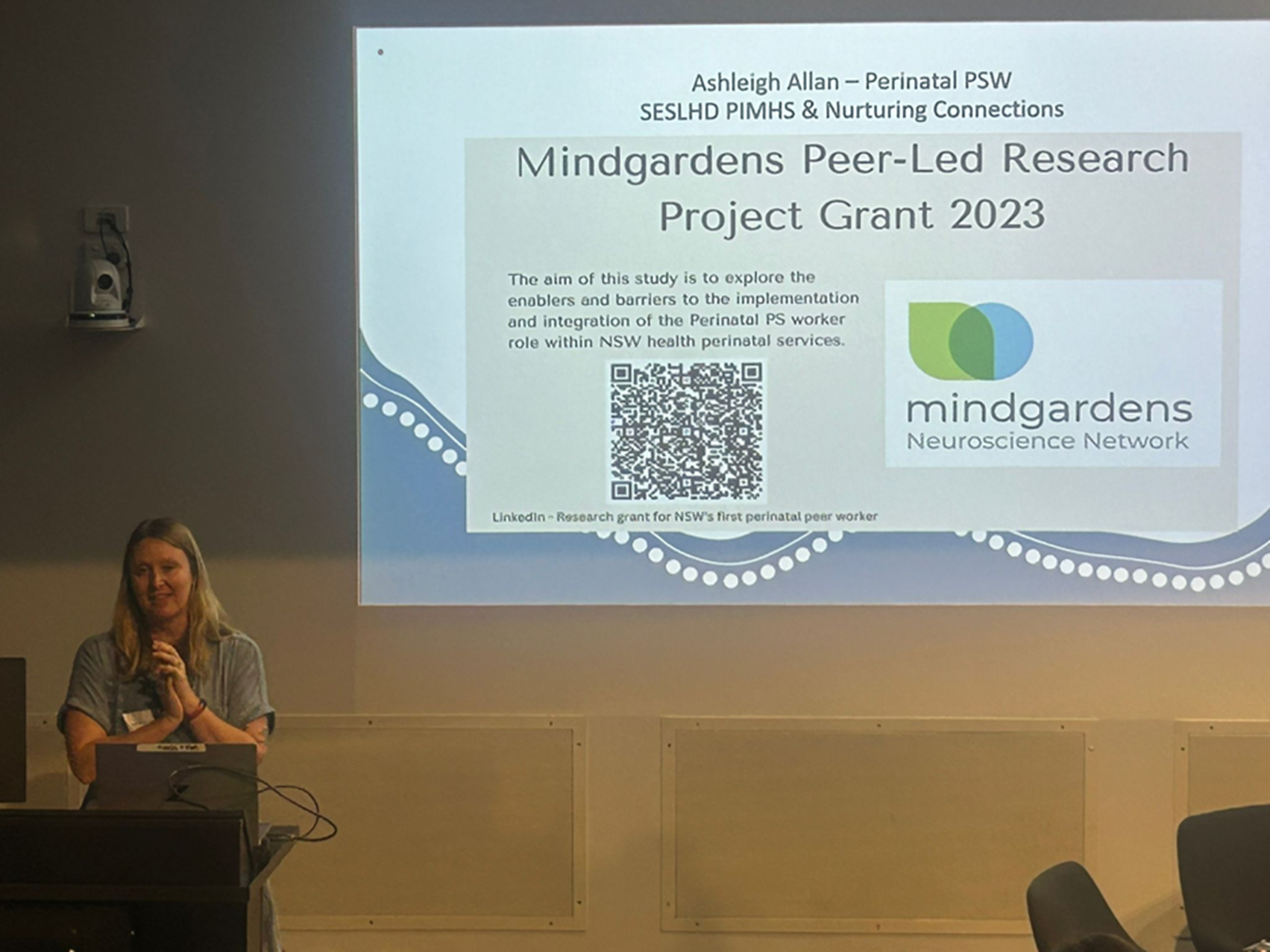
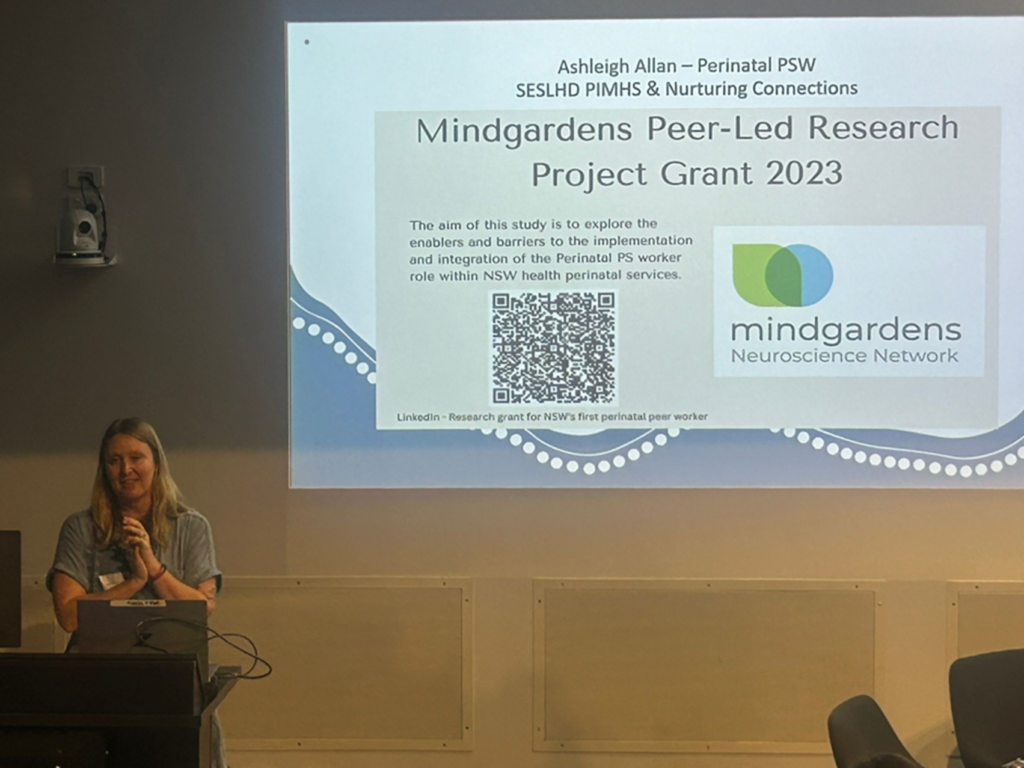
In November 2023, Ashleigh received the $10,000 Mindgardens Peer Led Research Program Grant, to study how perinatal peer support workers can be more fully integrated into perinatal and maternity services across NSW Health, with a focus on the perinatal peer support worker role within the SESLHD Perinatal & Infant Mental Health Service (PIMHS).
Ashleigh and Research Assistant Mary Burns interviewed SESLHD clinicians, consumers and members of the emerging perinatal peer workforce from across Australia, who enthusiastically shared their stories, and quickly exceeded their participant goals.
The interviews revealed participants felt unprepared for the experience of perinatal mental distress, with many having no previous experience of mental health concerns. The need for perinatal mental health support was often identified during pregnancy, with clinicians eager to refer consumers during the antenatal period as a form of early intervention and consumers open to referral to a perinatal peer support worker. Feelings of isolation and shame, and the stigma associated with them, can feel unique to the perinatal period, so access to a non-judgemental peer was welcomed. Continuity of care was also emphasised, with participants particularly valuing the relationship with an individual peer support worker.
More than 60% of participants stated they felt more confident as a parent as a consequence, with the peer worker giving them a safe space to reflect on their experiences. More than 80% felt more connected and accepted, reducing their feelings of isolation.
The researchers also drew on their own experiences and existing data, including findings from the Perinatal mental health in Australia, 2021-22 research undertaken by PANDA, which found that suicide is a leading cause of maternal death during pregnancy and the first year after birth; 20% of callers to the PANDA helpline experienced suicidal thoughts. One in five new mums experience perinatal mental health challenges each year, including around 600 who experience postpartum psychosis.
The Mindgardens grant allowed Ashleigh and colleagues to focus entirely on the research project for 12 months, building a case for a permanent peer support role within an experienced team. The research is now complete but this isn’t the end for Ashleigh’s project, with funding through PIMHS extended until June 2025, allowing Ashleigh and her team to formally evaluate the role and advocate for it to become permanently embedded within the PIMHS model of care.
There is strong international evidence for the unique value of peer support in recovery from mental distress, but the case for peer support in perinatal services is still emerging. Ashleigh’s findings are an important contribution, demonstrating the value of the perinatal peer worker role and how it enhances PIMHS services overall.
“The project was welcomed with open arms by the incredibly experienced mental health clinicians in the team,” Ashleigh said. “They’ve worked alongside peer workers and have a clear understanding of their value.” The team is now preparing a paper, which will describe the findings and how perinatal peer worker roles can be embedded within the PIMHS model of care.
Ashleigh paid tribute to the mentoring she received through Mindgardens alongside the grant, including the guidance of Dr Michael Hodgins from the University of New South Wales and support from Mindgardens Director of Lived Experience Catherine O’Donnell.
Mindgardens is proud to have helped Ashleigh “create a tangible evidence base for the role,” and we look forward to seeing her findings translated and applied, with more perinatal peer workers employed to support women in the transition to motherhood.
Project Team
Co-ordinating Principal Investigator: Ashleigh Allan
Organisation: SESLHD
Principal Investigator: Dr. Michael Hodgins
Organisation: Mindgardens & UNSW
Research Assistant: Mary Burns
Organisation: Mindgardens & UNSW
Supported by:
Mindgardens Team – Catherine O‘Donnell, Oliver Ardill-Young, Sarah Leung, Lyndall Truran
SESLHD Research & Ethics Team – Monique Macara & Caroline Cottet
PANDA – Perinatal Anxiety & Depression Australia
PIMHS – Perinatal & Infant Mental Health Service
Brings together the strengths of four founding organisations